Reprogram skin cells with gene therapy to better heal wounds
As we age, we have more and more trouble healing. Maybe you remember superficial wounds you got as a child. The healing was probably faster than that of your more recent wounds. And the phenomenon becomes more and more pronounced with age! Sometimes in the elderly, if the wound is too large, it cannot even close. The reason? Keratinocytes, the cells responsible for the formation of the outer layer of the skin, no longer migrate into the wound to repair it[1]. However, a study published in Nature may well provide a solution to this problem. Conducted at the Salk Institute for Biological Studies in La Jolla, California, this study shows that gene therapy can be used to transform wound cells into keratinocytes, and thus repair the wound from the inside.
Step 1: Identify the target genes for gene therapy

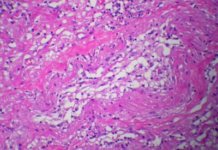
The principle of gene therapy is to use viruses to modify or express new genes within cells in a living being. But you still need to know which genes to use! The goal of the researchers is to find the genes to transform wound cells into keratinocytes. To find them, they start by comparing the gene expression profiles of these two cell types. They then identify 55 genes as potential targets.
By continuing their analyses, they managed to reduce this number to 28, which they then decided to test in-vitro. They express this cocktail of genes to cells similar to those of an open wound, and the results are there. If these cells are grown under conditions similar to those of the body, they form a structure similar to that of normal skin. But 28 genes is still too many to consider gene therapy. Then begins a laborious work where the experiment must be carried out again and again, removing each gene one by one to check if it is really essential. Finally, only 2 genes are essential, DNP63A and GRHL2, and two others greatly improve the efficiency of the transformation, MYC and TFAP2A.
Step 2: Check the effectiveness of in-vivo gene therapy
Now that researchers know the 4 genes they want wound cells to express, we still have to find a way to do it. As it is inconceivable to carry out these tests on humans directly, mice are chosen as guinea pigs. To carry out gene therapy, adenoviruses are chosen as carriers for genes. This is considered a safer option because their genome does not integrate into that of the cell they infect and therefore does not risk causing cancer.
The researchers inject different doses of virus including the 4 genes of interest into a skin wound in mice. They then noticed that for a sufficient dose of injected viruses, new skin would form to patch up the wound after 28 days. By analysing it, they discovered that it comes from wound cells transformed into keratinocytes by the viruses. In addition, this new skin shares the same properties as normal skin. The experiment is a success.

Last step: check that this gene therapy is safe

Gene therapy therefore works to heal wounds, but it could be risky for a number of reasons. The first is that viruses can infect and transform other cells in the body, which could be dangerous. By observing the mice treated with gene therapy, they observed that the viruses had affected both the injection site, as intended, as well as their liver. Although after dissection they did not observe any deleterious effects on them, they still decided to be more cautious. They then chose to replace the injection of the viruses with a hydrogel administration at the wound site. This also allowed them to incorporate growth factors that were supposed to boost healing. Once again, the experience was a success. The liver of mice was less affected and healing was even faster.
The second source of danger comes from the reprogramming of wound cells. In some cases, it can cause the formation of cells capable of forming tumours. To verify that this is not the case for their reprogrammed cells, the researchers carried out the following experiment. They injected mice without immune systems with either their reprogrammed cells, normal keratinocytes, embryonic stem cells known to form cancers under these conditions, or human cancer cells. They then observed that, as expected, embryonic stem cells and cancer cells formed tumours. However, their reprogrammed cells, like normal keratinocytes, did not form them. They could therefore conclude that their gene therapy is apparently safe.
Thus, gene therapy could be the solution to age-related scarring problems. As we have just seen, it would even be very effective and safe. This is reason to hope that research has once again enabled us to eradicate one of the consequences of aging in the near future!
References:
[1] Gurtner, G. C., Werner, S., Barrandon, Y. & Longaker, M. T. Wound repair and regeneration. Nature 453, 314–321 (2008).
[2] Kurita, M., Araoka, T., Hishida, T., O’Keefe, D. D., Takahashi, Y., Sakamoto, A., … & Hernandez-Benitez, R. (2018). In vivo reprogramming of wound-resident cells generates skin epithelial tissue. Nature, 1.
Baptiste Tesson

Author
Auteur
Baptiste is studying biology at the École Normale Supérieure de Lyon and bioengineering at the École Polytechnique Fédérale de Lausanne. He worked on the optimization of Cas9 as a tool for genome editing and on the emergence of blood stem cells in the zebrafish. He currently works on the patterning of the muscles, also in the zebrafish. He plans on doing a PhD in developmental biology.
More about the Long Long Life team
Baptiste étudie la biologie à l’École Normale Supérieure de Lyon et la bioingénierie à l’École Polytechnique Fédérale de Lausanne. Il a travaillé sur l’optimisation de la protéine Cas9 comme outil de modification de génomes et sur le développement des cellules souches du sang chez le poisson zèbre et travaille actuellement sur la mise en place des muscles chez le même animal. Il projette de réaliser un doctorat axé vers le développement animal.
En savoir plus sur l’équipe de Long Long Life



![[Video] Eurosymposium on Healthy Ageing, Brussels, 2018 Eurosymposium on Healthy Aging](https://www.longlonglife.org/wp-content/uploads/2019/07/P1310252-218x150.jpg)